Why would I need a Hysterectomy?
Usually this operation is only considered when other types of treatment to alleviate your symptoms have not been successful. The reasons for a hysterectomy can include:
-
Heavy or irregliar periods
-
Prolapsed uterus
-
Fibroids
-
Persistent Infection such as P.I.D (Pelvic Inflammatory Disease)
-
Painful pelvic adhesions and scarring
-
Persistent Endometriosis
-
Premenstrual Syndrome (PMS)
-
Cancer
-
In an emergency situation
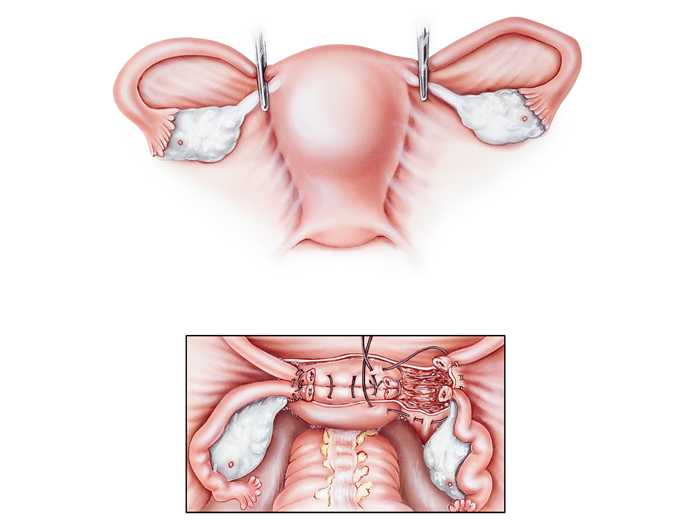
What are the different types of Hysterectomy?
-
Total abdominal hysterectomy – the removal of the uterus and cervix (neck of womb) whilst keeping the fallopian tubes and ovaries.
-
Total abdominal hysterectomy and Salpingo-oopherectomy – the removal of the uterus, cervix, fallopian tubes and ovaries.
-
Sub total abdominal hysterectomy – the removal of the uterus only, with the cervix being retained (some woman feel that the cervix is important for orgasm during sexual intercourse)
-
Radical hysterectomy or Wertheim’s hysterectomy – the removal of the uterus, cervix, fallopian tubes, ovaries, the upper third of the vagina and all of the lymph nodes in the region. (Usually performed when cancer cells have been found.)
These types of hysterectomy are performed through an abdominal incision, either vertically (mid-line) or transverse (bikini-line).
What are the advantages/disadvantages of an Abdominal Hysterectomy?
Advantages:
-
Clearer view of pelvic organs during surgery
-
More suitable if fibroids or scar tissue from previous surgery is present
-
More suitable if ovaries need removal at the same time
Disadvantages:
-
External scar
-
Recovery time slightly longer than with vaginal hysterectomy
-
Slightly higher risk of complications
Are there any risks involved?
Major surgery is safe and rarely results in complications. Your doctor believes that the benefits of treating your current problem with surgery outweigh the risks of such surgery. However the final decision as to whether or not you have the operation rests with yourself. In order for you to fully appreciate possible (albeit rarely) risks associated with such major surgery, we would like to explain them in more detail.
Haemorrhage (uncontrolled bleeding)
This is one of the most common complications during and immediately after surgery. You will be closely monitored so that any signs of haemorrhage should be detected and dealt with. At times of excess blood loss you may require a blood transfusion either during or after theatre. Very rarely you may need to be taken back to theatre to stop the bleeding.
Organ Damage
Very occasionally other pelvic organs may be injured during the operation, in particular your bladder or the tubes connecting kidney and bladder (ureters). This is usually rectified during surgery and only very rarely leads to permanent damage.
Possible Post-operative Complications
Deep Vein Thrombosis
A small number of women may develop a blood clot in their leg (deep vein thrombosis). In order to prevent this, the ward you are admitted to will use anti-embolic stockings, anti-coagulant injections and encourage early mobilisation. Occasionally such clots may travel around circulation and then block lung vessels (pulmonary embolism) which is life threatening. The risk of a DVT increases with age, smoking, the presence of cancer, history of blood clots, use of contraceptive pill, prolonged bed rest, obesity and the presence of varicose veins.
Urinary retention
Once your catheter has been removed you should pass urine normally within six hours. If you do not then another temporary catheter will be inserted to drain the bladder. The causes of retention are local pain and swelling of the urethra or a urinary infection.
Urinary Tract Infection
The insertion of a catheter during surgery may cause a urinary tract infection to develop. Symptoms may include pain when urinating, frequency, urgency, retention and concentrated urine. You will be treated with antibiotic if this is suspected.
Constipation
This is a common problem associated with surgery, often caused by medication and reduced mobility post-operatively. To help with constipation oral laxatives are prescribed.
To avoid the latter two complications it is advisable to drink 1-2 litres of fluid a day, and eat a balanced diet before surgery.
Wound Infection or Haematoma (Collection of blood under the skin)
If you develop a wound infection or haematoma you are likely to have a high temperature and a painful wound site. A wound swab will be taken and antibiotic therapy commenced. Very occasionally the wound site may break down and this will require further treatment in the form of dressings, and very rarely, surgery.
Pyrexia (High temperature)
If your temperature is higher than 38 degrees, it is likely you have an infection. A urine sample will be taken and blood samples collected to determine the cause of this infection.
Post-Op Instructions
-
No lifting/intensive exercise for 6 weeks
-
Gentle walking is okay
-
No sexual intercourse for 6 weeks
-
A vaginal discharge is normal for up to 6 weeks
Is it normal to feel weepy or depressed after a Hysterectomy?
Yes- It is a common reaction to the operation and being away from your family and friends. The return to normal life takes time and is a gradual process, however if these feelings persist when you leave hospital, the advice and support of your family, friends and hysterectomy/other women's support groups may help you. If you are concerned please contact your G.P.
Useful Support Groups
24 Hour helpline 0845- 4647